|
When silicone hydrogel (SiH) contact lenses were first launched in 1999, they were almost exclusively prescribed on an extended wear (EW) basis. Although it was clear that these new materials virtually eliminated the significant problems of hypoxia seen with EW of conventional hydrogel materials, it soon became clear that the EW of these lenses was by no means problem-free [1] [2] [3]. Additionally, epidemiological evidence now suggests that the incidence of severe corneal inflammatory events or microbial keratitis (MK) is similar for both EW SiH and EW conventional hydrogel materials [4] [5] [6], although the severity of these events may be reduced with SiH materials compared with conventional hydrogel materials [4]. Stapleton and colleagues [7] have recently published a comprehensive review on the epidemiology of contact lens related infiltrates and conclude that approximately one in every 500 EW soft lens wearers will develop presumed MK every year. Such observations have led to a renewed interest in SiH lenses for daily wear (DW).
The first SiH lens which was specifically formulated for DW was the Acuvue Advance lens (Johnson & Johnson) which was launched in 2004. This was soon followed by Acuvue Oasys (Johnson & Johnson) and O2 Optix (CIBA Vision) lenses. The Acuvue Oasys and the O2 Optix (or Air Optix) lenses are also approved for up to six nights of EW. The launch of these lenses is likely to be a significant factor in the plateau in the prescribing of SiH for EW and the concurrent increase in DW prescribing of SiH lenses which has been seen in various key markets around the world [8].
The case for daily wear
The literature is conclusive in demonstrating that overnight wear of all soft contact lenses increases the risk of developing MK compared with wearing them on a DW basis [7]. All forms of contact lens wear are known to alter the ocular defense mechanisms and disrupt the anterior ocular surface tissues, but these are intensified during overnight wear. Significant factors include the biochemical alteration to the tear film beneath a contact lens, exacerbated by stagnation of tears underneath it [9], entrapment of pathogens underneath the lens which have the capacity to alter the tear film and the corneal epithelial cells beneath them [9] and hypoxia-driven alterations to corneal homeostasis [10]. These factors are thought to be reduced (but not eliminated) in the DW situation mainly because of blinking and the reduced hypoxic load on the cornea. Recent epidemiological evidence suggests that hypoxia per se is not required for infection, but as Fleiszig states [9], it cannot be ruled out as a contributing factor.
Corneal inflammatory events
Wearing soft lenses, including SiH, on a DW basis significantly reduces the risk of MK. Epidemiological studies on the incidence of MK in soft lens DW prior to the launch of SiH lenses estimated that it occurred in the region of 2 to 7 per 10,000 (approximately one in every 2500 users per year) [7]. At present there is very little published data on the incidence of MK for DW in SiH lenses. Early data suggests that the incidence of severe infection may be higher with DW SiH lenses than with DW conventional soft lenses [5]. These data suggest that the annual incidence of MK (per 10,000 wearers) in DW SiH lens users is 4.5 compared with 0.9 in daily disposable lens users and 3.1 in DW conventional soft lens users. However, a recent case-control study in the UK [11] has found no significant difference in the relative risk of MK in DW SiH users, daily disposable users and DW planned replacement soft lens users. Perhaps contrary to what we as eye care practitioners would intuitively predict, the study found an increase in the risk of MK with daily disposable lenses compared with planned replacement soft lenses. However, the severity of disease was reduced in daily disposable lens users compared with planned replacement soft lens users. Additionally, the work suggests that there is increased risk for developing ‘sterile keratitis’ in DW SiH lens users (x 2.0) compared with users of planned replacement soft lenses [12].
Other adverse events
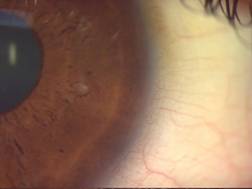
Hypoxia-related effects in DW have been virtually eliminated by SiH lenses and in this respect these materials are a significant improvement on their forerunners. The eye care practitioner now has a means of reversing the detrimental effects of hypoxia in existing lens wearers and crucially, prevent these effects developing in the first place. SiH lenses worn on a DW basis have been shown to induce significantly less limbal hyperaemia than conventional materials when fitted to neophytes on a DW basis [13] (Figure 1). Other studies have shown that limbal hyperaemia is significantly reduced in existing conventional soft lens wearers after being switched to DW SiH lenses [14]. This particular study also showed that wearers experienced improved end of day dryness and comfort after being switched to the SiH lenses.
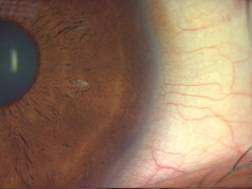
Since hypoxia is also known to be the primary cause of corneal vascularization, this is likely to be prevented in the long-term DW of SiH lenses. Long-term randomized trials are required in order to confirm this, but existing short-term clinical evidence supports this. The work of Dumbleton and colleagues [15] demonstrated that subjects who wore SiH lenses on an EW basis for nine months exhibited a reduced vascular response compared with subjects who wore lenses of lower oxygen permeability for the same period. Figure 2 shows neovascularization in a conventional soft toric wearer and subsequent emptying of the vessels following DW wear of a SiH toric lens. It is also reasonable to assume that there are likely to be minimal changes to the corneal endothelium and stroma as a result of long-term DW of SiH lenses, but as yet, we do not have the clinical evidence to support this.
 |
 |
| Figure 1. Increased limbal redness (right) in a neophyte subject following four weeks DW of a conventional soft lens. |
 |
 |
| Figure 2. Emptying of encroaching limbal vessels (right) in a DW subject re-fitted from a toric conventional lens to a SiH toric lens (four weeks DW). |
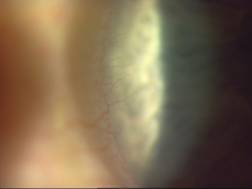
Other adverse events, such as contact lens papillary conjunctivitis (CLPC) and superior epithelial arcuate lesions (SEAL), which are associated with SiH contact lenses have been previously well documented on this website. The incidences of these adverse events have received much attention in EW, but they are also encountered during DW (Figure 3). The recent UK case-control study outlined above reported that DW SiH users are 2.8 times more likely to develop papillary conjunctivitis than users of daily disposable lenses and this is presumably related to the greater stiffness of SiH materials compared with conventional hydrogels. However, this difference fell just short of the level required for statistical significance [12].
 |
 |
| Figure 3. ‘Pre-SEAL’ (left) and SEAL (right) in two different subjects wearing SiH lenses on a DW basis. |
Comfort and lens surface wettability
At present there is no conclusive evidence that comfort during DW is significantly different with SiH lenses compared with conventional hydrogels. Some studies have reported improved comfort with SiH lenses compared with conventional soft lenses [14] [16], whilst other studies have failed to show a difference [17]. Despite the introduction of care systems which have been specifically formulated to enhance SiH lens comfort, a lens or a lens/solution combination, which maintains its comfort throughout the day, still eludes us.
The increased hydrophobicity of SiH lens surfaces compared with conventional hydrogel surfaces has been the focus of much clinical and laboratory research. These surfaces have been shown to deposit low levels of protein (which is largely denatured), but relatively high levels of lipid [18]. This has resulted in wettability-related problems in a number of wearers [13] which can also impact on vision and comfort. A combined rub and rinse step used in conjunction with multipurpose solutions has been shown to significantly reduce this deposition [19].
Contact lens care systems
All SiH lenses worn on a DW basis currently require the use of a care system since there is currently no daily disposable SiH lens on the market. Recently, there has been much interest in the level of ‘compatibility’ (as evidenced by the level of so-called corneal ‘toxicity’ staining) of various solution/lens combinations, with particular interest in the SiH materials [20]. In addition, the recent withdrawal of two multi-purpose contact lens solutions from the market has highlighted the issue of whether we can continue to realistically marry convenience and disinfection effectively, in a single step. There is now strong evidence to suggest that hydrogen peroxide disinfection produces the lowest levels of corneal staining when used with hydrogel lenses. Reducing the levels of corneal staining in contact lens wearers is important as there is recent evidence that corneal staining is associated with the development of corneal infiltrates [21] [22].
Compliance
Morgan [23] has recently presented the results of a web-based compliance questionnaire and has outlined how poor compliance can shift the balance between bioburden and ocular defense mechanisms and in doing so, potentially increase the risk of inflammation and infection in the cornea. Contact lens compliance was evaluated for 1,402 wearers of planned replacement lenses (two or four weekly replacement) in seven European countries. The study found that only 0.3% of lens wearers were fully compliant in all areas investigated for DW compared with 2.7% for EW. Morgan concluded that the areas where improved compliance should lead to reduced risk of significant and serious keratitis included not sleeping in DW lenses, discarding them at the correct interval, rubbing as well as rinsing lenses, cleaning the lens case after each use and allowing it to air dry and thorough hand washing before lens handling. The next challenge will be how to get across better public service messages and how we, as eye care practitioners, can ensure we deliver more effective patient instruction and education.
Summary
SiH materials provide enough oxygen to the cornea during DW to eliminate both the short-term and, in all likelihood, the long-term effects that are seen with conventional hydrogel materials as a result of hypoxia. In this respect there is no doubt that they represent a significant improvement from conventional hydrogel materials. However, the introduction of SiH lenses has brought along its own, new set of complications principally related to the mechanical characteristics of these materials and the wettability of these inherently hydrophobic surfaces. The indication that the incidence of MK remains similar for DW SiH lenses and DW soft conventional lenses means that we must continue in our efforts to understand the pathogenesis of this disease and continue to improve the biocompatibility of future materials.
References
- Dumbleton KA. Noninflammatory silicone hydrogel contact lens complications. Eye & Contact Lens 2003; 29: S186-S189.
- Morgan PB, Efron N, Maldonado-Codina C et al. Adverse events and discontinuations with rigid and soft hyper Dk contact lenses used for continuous wear. Optom Vis Sci 2005; 82: 528-535.
- Millar TJ, Papas EB, Ozkan J et al. Clinical appearance and microscopic analysis of mucin balls associated with contact lens wear. Cornea 2003; 22: 740-745.
- Morgan PB, Efron N, Hill EA et al. Incidence of keratitis of varying severity among contact lens wearers. Br J Ophthalmol 2005; 89: 430-436.
- Stapleton F, Edwards K, Keay L et al. The incidence of contact lens associated microbial keratitis in Australia. Invest Ophthalmol Vis Sci 2005; 46: E-abstract 5025.
- Schein OD, McNally JJ, Katz J et al. The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology 2005; 112: 2172-2179.
- Stapleton F, Keay L, Jalbert I et al. The epidemiology of contact lens related infiltrates. Optom Vis Sci 2007; 84: 257-272.
- Morgan PB. Is daily wear the principal use for silicone hydrogel materials? http://www.siliconehydrogels.org Editorial, December 2005.
- Fleiszig SM. The Glenn A. Fry award lecture 2005. The pathogenesis of contact lens-related keratitis. Optom Vis Sci 2006; 83: 866-873.
- Stapleton F. Silicone hydrogel contact lenses and the ocular surface. The Ocular Surface 2006; 4: 24-43.
- Dart JKG. Epidemiology of microbial keratitis - have silicone hydrogels had any impact? Lecture presentation at the BCLA Clinical Conference and Exhibition, Manchester, UK. May 31-June 3, 2007.
- Radford CF, Stapleton F, Verma S et al. Case-control study of non-ulcerative contact lens complications in an ophthalmic accident and emergency department. Poster presentation at the BCLA Clinical Conference and Exhibition, Manchester, UK. May 31-June 3, 2007.
- Maldonado-Codina C, Morgan PB, Schnider CM et al. Short-term physiological response in neophyte subjects fitted with hydrogel and silicone hydrogel contact lenses. Optom Vis Sci 2004; 81: 911-921.
- Dumbleton KA, Keir N, Moezzi A et al. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci 2007; 83: 758-768.
- Dumbleton KA, Chalmers RL, Richter DB et al. Vascular response to extended wear of hydrogel lenses with high and low oxygen permeability. Optom Vis Sci 2001; 78: 147-151.
- Young G, Riley CM, Chalmers RL et al. Hydrogel lens comfort in challenging environments and the effect of refitting with silicone hydrogel lenses. Optom Vis Sci 2007; 84: 302-308.
- Cheung SW, Cho P, Chan B et al. A comparative study of biweekly disposable contact lenses: silicone hydrogel versus hydrogel. Clin Exp Optom 2007; 90: 124-131.
- Lorentz H, Jones L. Lipid deposition on hydrogel contact lenses: how history can help us today. Optom Vis Sci 2007; 84: 286-295.
- Nichols JJ. Deposition rates and lens care influence on galyfilcon A silicone hydrogel lenses. Optom Vis Sci 2006; 83: 751-757.
- http://www.staininggrid.com
- Carnt N, Jalbert I, Stretton S et al. Solution toxicity in soft contact lens daily wear is associated with corneal inflammation. Optom Vis Sci 2007; 84: 309-315.
- Carnt N, Keay L, Naduvilath T et al. Risk factors associated with corneal inflammation in soft contact lens daily wear. Invest Ophthalmol Vis Sci 2007; 48: E-abstract 4326.
- Morgan PB. Contact lens compliance and reducing the risk of keratitis. Optician 2007; In press.
|