Contact-Lens-Induced Conjunctival Epithelial Flaps: What Are They and Do We Need to Worry?
A relatively new clinical finding, referred to as “conjunctival epithelial flaps” (CEF), occurring with silicone hydrogel lenses, was recently reported [1,2]. This term is used to describe conjunctival epithelium splitting from its underlying tissue which might sheath the neighboring conjunctiva. This diagnosis is made easier after instillation with fluorescein and examination of the conjunctiva with a yellow filter in conjunction with a cobalt blue light illuminating system. Loose tissues associated with conjunctival epithelial flaps become apparent as fluorescein dye pools under the flap.
Conjunctival epithelial flaps are usually found approximately 0.5 mm away from the soft lens edge in superior and/or inferior quadrants. The jagged edge associated with the flap usually marks the limit of vertical movement of the silicone hydrogel lens. Although conjunctival epithelial flaps can be accompanied by lens indentation or conjunctival epithelial disruptions highlighted by fluorescein or rose bengal staining, the incidence rate or the extent of this phenomenon is not associated with severity of conjunctival staining.
The appearance of a conjunctival epithelial flap varies based on the lens wearing modality; the sizes of the flaps range from 0.1 to 0.5 mm in daily wear (Figure 1) and are considerably smaller than those observed during continuous wear (~ 9 mm) (Figure 2).
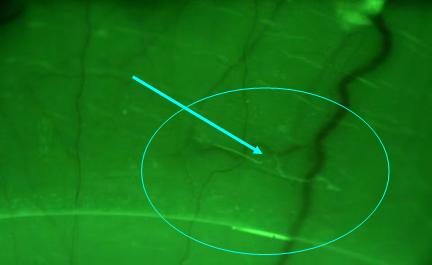 |
| Figure 1 - Arrow denotes a small conjunctival epithelial flap in daily wear |
| |
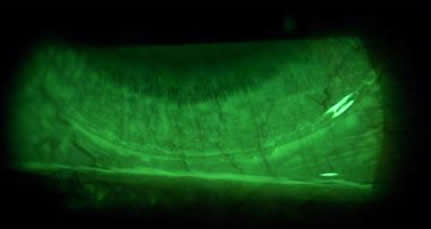 |
| Figure 2 - Conjunctival epithelial flap in continuous wear (courtesy of Tom Løfstrøm) |
Recent studies show that conjunctival epithelial flaps occur at a rate of about 3% of daily wearers and in about 37% of continuous wearers [1, 2]. In most reported cases, wearers are asymptomatic. The etiology of this condition has not yet been determined. However, it is possible that in addition to lens wearing modality, higher modulus lens materials along with a non-rounded edge design can increase the risk of an event occurring. The recovery time after lens cessation depends on the extent of the flap; a small lesion (~ 0.5 mm) takes a minimum of 24 hours to resolve, whereas larger flaps (~ 9.0 mm) can take several weeks. Preliminary analysis of an ongoing study at the University of California, Berkeley Clinical Research Center (UCB-CRC) has shown that this condition has no age and gender predilection. However, Asians seem more likely to have the condition possibly due to the presumed higher lid tensions, which may increase mechanical irritations on the ocular surface during contact lens wear.
Of interest, in the “fresh” occurring cases (< 7 days of continuous wear), there is no clinical sign of rose bengal staining, possibly suggesting that conjunctival flaps are composed of vital cells. A recent study using impression cytology with cellulose acetate filters also shows that after 1-week of continuous wear those cells are not devitalized [3]. However, researchers at UCB-CRC have observed that conjunctival cells after 30-days of continuous wear stain brightly with rose bengal dye while in the same wearers, no staining is observed after 7-days of continuous wear. These stained cells are either devitalized or simply stain because of insufficient mucin protection. Nevertheless, this result suggests that continual mechanical irritation due to either lens material (high vs. low modulus) and/or lens edge design (sharp vs. round) can increase the incidence of conjunctival flaps.
There are many questions that remained unanswered:
- In the long-term, do conjunctival epithelial flaps cause a decrease in goblet cell density?
- In the long-term, do conjunctival epithelial flaps cause a decrease in lens-wearing comfort?
- When the loose tissues or flaps get dislodged, can these remnants become trapped underneath a silicone hydrogel lens and trigger immunological responses, especially when we know that these lenses still do not have efficient post-lens tear exchange?
- Can potentially harmful microorganisms become trapped within “pockets” of loose conjuctival flaps, leading to increased risk of surface infection?
Future studies are needed to elucidate the long-term clinical relevance and the pathogenesis of this conjunctival tissue response to silicone hydrogel lenses.
Clearly, we have more questions than information. Since the advent of silicone hydrogels, hypoxic-induced adverse events have virtually been eliminated. Unfortunately, complication rates have not decreased. Clinicians should continue to carefully examine the health of the ocular surface. Although conjunctival flaps appear to be benign from a wearer’s perspective, it involves a mechanical disruption of the ocular surface and any potential long-term effects are not fully understood. Fortunately, this condition can be completely eliminated simply by switching lens materials and/or designs as well as by changing lens-wearing modality.
Reference:
- Løfstrøm and Kruse. Contact Lens Spectrum. September 2005.
- Lin, Truong, Thota et al. AAO abstract. December 2005.
- Thota, Perrigin, Miller et al. ARVO abstract. May 2006.
|