At a recent Symposium, Brien Holden, on behalf of Vision Cooperative Research Centre (VisionCRC), LVPEI
and CCLR colleagues and teams, gave some of the suggestions
and measures that have been drawn up to minimise the risk of
microbial keratitis and, if such an event arises, to treat
a suspected MK event.
Though this is preliminary information that may form the basis
of a publication or publications on the issue, we thought it
would be of value to pass the information on in this form.
Desmond Fonn and Debbie Sweeney
  
MK Diagnosis
The accurate diagnosis of Microbial Keratitis (MK) is vital,
as significant delay in treatment or inappropriate treatment
can seriously affect the visual outcome.
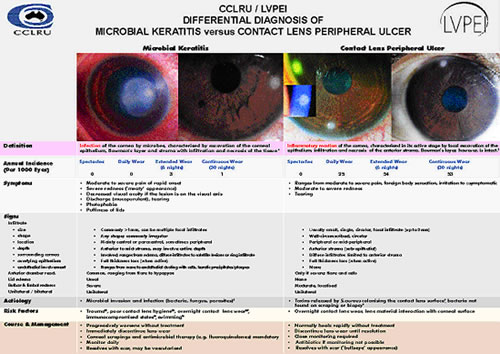
Vision Cooperative Research Centre (VisionCRC) and LVPEI have developed a differential diagnosis protocol
to assist practitioners in the diagnosis of CLPU and MK. CLPU
is often mistaken for MK, and this guide will provide practitioners
with a clear analysis of the different signs and symptoms, and
a step by step checklist to guide diagnosis.
This guide, shown here, will soon be available from Vision Cooperative Research Centre (VisionCRC).
Differential Diagnosis of CLPU v MK

MK: Treatment Strategy
MK treatment should immediately follow diagnosis. The initial
empiric antibacterial treatment options for typical causative
organisms (Pseudomonas aeruginosa, staphylococcus species,
Streptococcus Pneumoniae) are:
- Topical Fluroquinolone (e.g. ciprofloxacin 0.3%, ofloxacin
0.3%) monotherapy (not in documented or suspected streptococcal
keratitis)
- 2 drops/15min for 6 hours
- 2 drops/30 mins for 18 hours
- 2 drops/60 mins for 24 hours
- 2 drops/2hours for days 3 and 4 (day only)
- Topical Fluroquinolone (eg ciprofloxacin 0.3%, ofloxacin
0.3%) + topical fortified Cefazolin (50mg/ml) (preferred
agent for Gram positive coverage: if there is a possibility
of streptococcus
pnueumoniae, or resistant Gram positive organisms)
- As above
MK: Therapeutics
Initial treatment should be topical fortified Tobramycin (13.6mg/ml)
+ topical fortified Cefazolin (50mg/ml) (preferred agent for
Gram positive coverage):
- Give first doses (a “loading dose”): 1
drop every minute for 5 minutes
- Use topical fortified antibiotic A every hour (on the hour)
- Use topical fortified antibiotic B every hour (on the half
hour).
- After 36-48 hours:
- reduce therapy if clinical improvement occurs
- use topical fortified antibiotic A every 2 hours
- topical antibiotic B is either discontinued or used every 2 hours,
5 minutes after antibiotic A.
- After 48-72 hours:
- use topical fortified antibiotic A every 3 to 4 hours
- use antibiotic ointment at bedtime
- discontinue medication after bedtime.
- After 96+ hours:
- change to regular-strength antibiotic drops and slowly taper
off this medication
- continue antibiotic ointment at night for approximately 1 week.
In the Practice
To protect your patients and your practice, it is important
that standard operating procedures are followed for infection
control. Typical guidelines for such procedures can be found
at:
The following guidelines should be standard procedures within
any practice to help to prevent infection. These should be followed
as a matter of course, not just in the case of MK or other adverse
event.
Handwashing
Within the practice and for the patient, handwashing is still
the MOST important procedure to stop the spread of infections.
- Hands must be washed prior and post to seeing any patient
- Hand wash should take at least 10 seconds
- Remove jewelry
- Use running water and 2% chlorhexidine gluconate
- Use friction/rubbing action
- Wash all areas
- Hands are to be rinsed well and dried completely with lint
free ‘tissues
- Use non-perfumed, hypo-allergenic hand creams to avoid cracking
of skin or dermatitis.
Gloves
Gloves should be used whenever there is contact with tears or
contact lenses:
- Hands must still be washed before gloves are worn and
after they have been removed
- Use non powdered gloves
- Vinyl gloves may be used. Ensure these fit well.
Instruments
Clinical facilities must also be kept clean and free from infection.
- Work benches must be cleaned using a neutral soap solution.
- Instruments that do not come into direct contact with a patient’s
eye (e.g. chin rests) should be cleaned between patients,
using a neutral soap solution.
- Instruments that do come into contact with eyes (e.g. tonometer)
should be disinfected. Tonometer prisms disinfected by a 5-minute
soak in 3% hydrogen peroxide (or 70% isopropyl alcohol or a
1:10 dilution of sodium hypochlorite) are adequately disinfected against
most ocular pathogens, with the exception of Acanthamoeba.
Lenses
- Autoclave any lens that is to be re-used OR
- Disinfect with a 2-hour soak in 3% hydrogen peroxide.
- After disinfection, rigid lenses should be stored dry, and soft
lenses should be stored in a sterile, preserved solution.
- Repeat disinfection should be routinely performed at 1-month
intervals to prevent regrowth of organisms.
Infection Control
Particular care should be taken with ALL adverse reaction/red
eye patients:
- All staff (Optometrists, Clinical Assistants and any
other staff coming in direct contact) should use gloves for entire
consultation, disinfecting or discarding procedures.
- A designated room should be used for any adverse event patients.
- Any patient presenting with a red eye should be seated in this
room rather than being asked to wait in waiting area (if practical).
- Disinfect / discard any items handled by adverse event patients.
Patient Management
Aftercare Visits
Regular checks of all contact lens patients will ensure timely
identification of any problems, and will also remind patients
of the care schedules and procedures, and of the importance
of daily checks of their eyes.
New lens patients should be seen:
- after one week
- after first month
- after three months
- then every three to six months.
Management of Adverse Ocular Responses
For the practitioner, accurate diagnosis of adverse events is
key to their appropriate management, identification of risks,
and prevention.
For the patient, it is important that they:
- are aware of how to minimise the risk of adverse events
- check their eyes daily and can recognise warning signs
- seek help promptly if any problems arise.
Patient education should continue at every practice visit to
reiterate these points.
Minimising The Risk Of Adverse Events
 Hygiene and general lens care should also be emphasized at every
visit. Hygiene and general lens care should also be emphasized at every
visit.
- If a contact lens is out of the eye for any time, it
should be disinfected before replacement in the eye, or a new
lens should be used.
- Patients should be encouraged to use lubricants (a sterile unit
dose), particularly in the morning upon waking, and in the evening.
Most recently, swimming in contact lenses has been identified
as a risk factor in MK. Practitioners should recommend to their
patients that they wear goggles whenever they swim. An information
and reminder sheet is available here for downloading and printing,
for distribution to your contact lens patients.
One of the most important guidelines for patients is:
 Don’t sleep with the lenses on when: Don’t sleep with the lenses on when:
- The eye is red
- The eye is sore or irritated
- You are generally unwell/sick
- sore throat
- influenza
- Or if you have others sick in your household
Checking Their Eyes Daily
 Each day, patients should check to see if their eyes: Each day, patients should check to see if their eyes:
- Look good
- Feel good, and
- See well.
Patients should be told that if their vision is blurry, or if
there is any irritation, they should:
- Remove the lens
- Rub and rinse
- Return the lens to eye
- If there is no improvement
- Try a spare lens
- If there is no improvement
- CONTACT THE CLINIC
Patients should be encouraged to always have an up-to-date spare
pair of spectacles to use.
Contacting The Practitioner Promptly
Patient should be encouraged to contact their practitioner IMMEDIATELY
there is a problem.
This will be important to ensure accurate diagnosis and treatment
of any problems.
Wherever possible practitioners should provide 24 hour emergency
phone numbers. 
|