Epidermolysis Bullosa (EB) is a rare inherited disease in which the most minor trauma causes the skin to blister. Patients with EB are likely to develop corneal lesions, which can adversely affect the vision. Dystrophic EB is a more severe form of the condition, where the corneal epithelium is abnormally attached to the basement membrane. Patients with dystrophic EB are also at risk of symblepharon.
Severe corneal problems are relatively infrequent but when they do occur, they can be difficult to manage. Large corneal erosions and abrasions can be of sudden onset and cause a great deal of pain and photophobia. This is usually managed with ocular lubricants and occasionally with therapeutic contact lenses (TCLs). Great care is needed when fitting lenses to the compromised cornea. Until relatively recently, hydrogel lenses were fitted but since the lenses need to remain in place for several days, the risk of hypoxia is now much reduced by fitting Silicone hydrogel TCLs.
A young female patient with dystrophic EB was first seen at the age of 6 years in the hospital ophthalmology department. She had been in and out of hospital from a very early age for her severe skin problems. When she first presented, she was complaining of pain in her Left eye. On examination, she was found to have lesions and blisters. The eye was treated with regular lubricating drops and ointment and it improved slowly but result in lesions and central scarring (Figure 1) leading to irregular corneal astigmatism and amblyopia and the best corrected vision was 0.60 logMAR (6/24). The Right eye remained clear and the vision was 0.04 (6/6-) unaided.
Over the next few years, the Left eye continued to have problems but at the age of 11 years, the Right eye developed a corneal ulcer leading to a full thickness corneal perforation and a flat anterior chamber. An Air Optix Night & Day lens 8.60/13.80/-0.50 was fitted as a TCL in an attempt to try to reform the anterior chamber. The vision in that, her better eye, had dropped to HM only and the iris had not reformed by the next day. She therefore underwent an emergency procedure to glue the cornea with cyanoacrylate glue, and a similar TCL was inserted to protect the eyelid.
The low water content and relatively high modulus of an Air Optix Night & Day lens helps it to withstand the irregular surface of the glue and maintain comfort while the anterior chamber has the chance to reform. This treatment was effective and the lens remained in place until she had a corneal transplant 4 days later. Unfortunately, whilst the anterior chamber was flat, she had developed posterior synechiae and she required a lensectomy and vitrectomy at the same time.
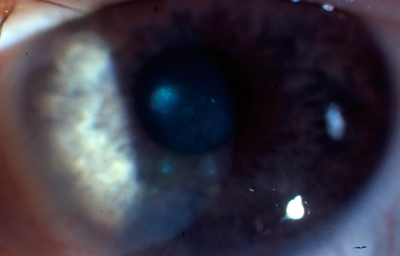
The eye recovered slowly and she was prescribed aphakic spectacles for the Right eye (+17.00/-2.50x30 V/A 0.4 logMAR (6/15)). She found this difficult to cope with especially with the reduced mobility resulting from her general condition. When it was judged safe to fit a lens, even though the corneal sutures had not been removed (Figure 2), a Silicone hydrogel lens (Ultravision Hydrowave 8.30/14.20/+18.50) was ordered.
The patient was keen to handle the lens herself but had great difficulty removing this lens because of the damage to her fingertips caused by the EB blisters, so her mother helped initially. With a bifocal spectacle overcorrection (Plano/-3.00 x 160 Add +3.00), she is able to see 0.0 logMAR (6/6) in the distance and can read N5 at 30cm. Over the course of a year's follow up, she has had no neovascularisation and minimal stain.
Possibly as a result of the problems in the Right eye, the vision in the amblyopic Left eye improved with spectacle correction to 0.40 logMAR (6/15). She was getting on so well with the Right lens that it was decided that it would be worthwhile fitting the Left eye with a lens as well. A disposable silicone hydrogel lens (Acuvue Oasys for Astigmatism 8.60/14.50/ -1.25/-1.75 x 30) was ordered.
The Left eye is at high risk of developing neovascularisation because of the central scarring and a hydrogel lens would not be advisable. Indeed, an even higher Dk silicone hydrogel would be preferable and was tried but the patient did not find it comfortable.
Now aged 13 years, she wears both lenses most of the day and can handle them herself. She continues to use drops in both eyes and is reviewed every 3 months.
Figure 1: Corneal lesions and central corneal scarring
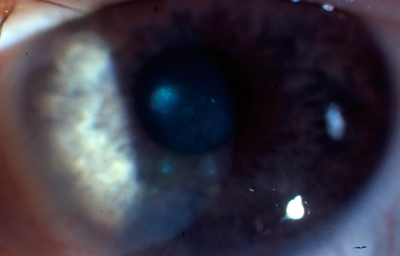
Figure 2: Corneal graft with the sutures still in situ. Anterior synechiae have formed in the 9 o'clock position
|