Introduction
Contact lens papillary conjunctivitis (CLPC) was first reported by Spring in 1974 and is described as a reversible, inflammatory reaction of the upper palpebral conjunctiva (UPC). [1] It is characterised by enlarged papillae >0.3 mm, palpebral hyperaemia and mucus secretion. [2, 3] While CLPC is a non-sight threatening, reversible condition, symptoms include itching and ocular discomfort which can lead to contact lens (CL) intolerance and discontinuation of wear. [4] Treatment strategies advocate reduced wear time and frequent replacement of lenses.
Incidence of CLPC
The suggested incidence of CLPC varies widely in the literature and has been reported as between 1.5 (Lamer 1983) and 47.5% (Alemay and Redal 1991). Studies performed during my recent research (PhD thesis 2007) indicate a CLPC rate of 4.6 % for wearers of first generation silicone hydrogels (SiHis).
The increasing use of silicone hydrogel lenses with their potential to be used on an extended wear basis may lead to an increased incidence of CLPC. This article will review clinical presentations and the aetiology of CLPC with high Dk SiH lenses.
Two different presentations of CLPC
In order to examine the aetiology of CLPC, a detailed description of the presentation is required. Firstly, the area of the tarsal plate affected should be differentiated. This can be achieved by following the direction of Allansmith et al (1977) [2] who separated the palpebral conjunctival area into 5 discrete zones (Figure 1). Secondly, the distribution of the papillae can be described in accordance with Holden et al (2000) who suggested that it is possible to separate CLPC into two different presentations; either ‘local’ or ‘general’. ‘Local’ is defined as papillae confined to one or two areas of the upper palpebral conjunctiva and ‘general’ if papillae are scattered across three or more areas. [10]
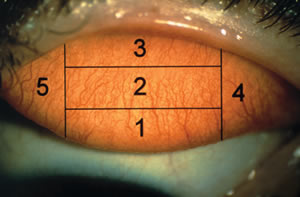 |
| Figure 1: Five zones of the upper palpebral conjunctiva of the right eye |
During this investigation, both the position and distribution of papillae were examined to obtain a detailed evaluation of the presentations of CLPC with high dk SiH wearers. Several aspects of lens wear were compared, including: patient and lens characteristics, and distribution of clinical presentations of enlarged papillae between local and general types at two clinical sites (Vision CRC in Sydney, Australia from 1998 to 2004 and LV Prasad Eye Institute in Hyderabad, India from 1993 to 2003).
Differences in the location and number of areas involved between local and general CLPC presentations were confirmed. The enlarged papillae and hyperaemia manifest most often in zones 2 and 3 of the UPC in local cases of CLPC (Figure 2), whereas, in general CLPC, the majority were observed in zones 1, 2 and 3 and sometimes in zones 4 and 5 (Figure 3). The incidence of local CLPC was found to be 3.4% compared to 1.2% for general cases of CLPC. These results are significantly different and strongly suggest that the aetiology of the two presentations may differ. The data also indicates that the majority of CLPC cases in high Dk SiH lens wearers are associated with the local response.
The symptoms reported between the two groups were similar, with blurred vision, lens awareness, eye secretion and itching most frequently described. Mean lens centration, movement and tightness were optimal for local and general presentations. No clinically significant differences were found for lens wettability between local and general cases and asymptomatic controls, however, front surface deposits were clinically greater in both cases compared to asymptomatic controls. No differences in patient characteristics such as mean age and gender were observed between the two types of presentations.
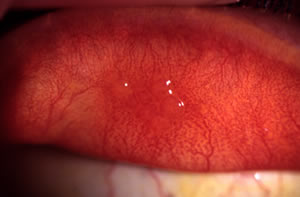 |
| Figure 2: An example of a case of local CLPC at 16x mag. Note enlarged papillae in zone 2 of the upper palpebral conjunctiva |
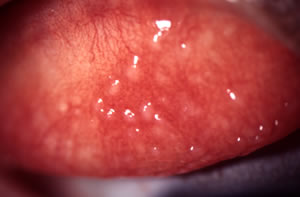 |
| Figure 3: An example of a case of general CLPC at 16x mag. Note enlarged papillae in zones 1, 2 & 3 of the upper palpebral conjunctiva |
Aetiology
The two presentations lead us to believe that there may be differences in aetiology.
- High Dk SiH lenses have a higher modulus of elasticity (1.1-1.2 MPa) making the lens stiffer than hydrogel lenses [11]. The stiffness of the lens material may contribute to mechanical irritation of the lens rubbing against the UPC producing a local response. The lens and edge design may also promote mechanical irritation to the upper lid.
The influence of lens design on the development of local CLPC is demonstrated by the difference in incidence between spherical and aspheric lens designs. Aspheric lens wearers show less local CLPC than those wearing spherical lenses (4.4% vs 1.8%, respectively). This maybe as an aspheric lens approximates the shape of the cornea more closely so that there is less lift-off over the periphery of the cornea and limbal areas.
- The distribution of papillae in general CLPC may indicate an immunological response initiated by the deposits or allergens that accumulate on the contact lens surface. [2, 12-13]. The resulting mechanical interaction between deposits rubbing against the UPC encourages the development of general CLPC.
- CLPC has been reported to occur more frequently with silicone hydrogel CW than with conventional lens wear.[14] The changes that occur in overnight wear may include some or all of the following: tear stagnation, localized pressure, closed eye environment producing a sub clinical inflammatory condition and frictional rubbing of the lens on the UPC [15-16]. We can speculate that some or all of the changes in the UPC contribute to the subsequent development of CLPC.
CLPC and new high Dk lens materials
With the introduction of the lower modulus/second generation SiH lenses, what will be the affect on the incidence of CLPC?
Recent studies indicate a lower incidence of CLPC with the lower modulus lens formulations and the option of a second steeper base curve.[14]. Further follow-up is needed to investigate whether it is the incidence of local CLPC that has changed, which is perhaps more likely than a different rate of general CLPC. [17]
The popularity of high Dk silicone hydrogel lenses will continue to grow as improvements to the lens designs, materials and surface properties continue. These changes and use of DW modality in those susceptible patients should bring about a significant reduction in the incidence of CLPC.
References
- Spring TF (1974)Reaction to hydrophilic lenses. Med J Aust.,1: 449-450
- Allansmith MR, Korb DR, Greiner JV, Henriquez AS, Simon MA, Finnemore VM (1977). Giant papillary conjunctivitis in contact lens wearers. Am J Ophthalmol 83(5):697-768.
- Korb DR, Allansmith MR, Greiner JV, Henriquez AS, Richmond PP, Finnemore VM (1980). Prevalence of conjunctival changes in wearers of hard contact lenses. Am J Ophthalmol 90:336-341.
- Allansmith MR, Ross RN (1989). Early stages of giant papillary conjunctivitis. Cont Lens J 17:109-114.
- Holden BA, Sankaridurg PR, Jalbert I (2000) Adverse events and infections. In: Silicone Hydrogels: Continuous wear contact lenses. 2nd edition, 2004. Butterworth Heinemann. Oxford, UK. pp. 251
- Lamer L. (1983) EW contact lenses for myopes: a follow-up study of 400 cases. Ophthalmology, 90:156-161
- Alemay AL and Redal P (1991). Giant papillary conjunctivitis in soft and rigid lens wear. Contactologica, 13: 14-17
- Nilsson S (2001). Seven-day extended wear and 30-day continuous wear of high oxygen transmissibility soft silicone hydrogel contact lenses: a randomized one-year study of 504 patients. CLAO J 27:125-136.
- Skotnitsky c, Sankaridurg PR, Sweeney D, Holden BA, (2002) General and local contact lens induced papillary conjunctivitis (CLPC). Clin Exp Opt 85(3): 193-7.
- Holden BA, Sankaridurg PR, Jalbert I (2000) Adverse events and infections. In: Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses (D Sweeney, ed.), Butterworth Heinemann, Oxford, UK, pp.150-213.
- Tighe BJ (2000). Silicone hydrogel materials – how do they work? In: Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses (D Sweeney, ed.), Butterworth-Heinemann, Oxford, pp. 1-21.
- Allansmith MR (1989). Immunologic effects of extended-wear contact lenses. Ann Ophthalmol 21;465-474.
- Ballow M, Donshik PC, Rapacz P, Maenza R, Yamase H, Muncy L (1989). Immune responses in monkeys to lenses from patients with contact lens induced giant papillary conjunctivitis. CLAO J 15;64-70.
- Dumbleton, K., Noninflammatory silicone hydrogel contact lens complications. Eye & Cont Lens, 2003. 29(1 Suppl): p. S186-9; discussion S190-1.
- Sack RA, Sathe S, Hackworth LA, Willcox MD, Holden BA, Morris CA (1996). The effect of eye closure on protein and complement deposition on Group IV hydrogel contact lenses: relationship to tear flow dynamics. Curr Eye Res 15;1092-1100.
- Sack RA, Tan KO, Tan A (1992). Diurnal tear cycle:evidence for a nocturnal inflammatory constitutive tear fluid. Invest Ophthalmol Vis Sci 33:626-640.
- Maldonado-Codina C, Morgan PB, Schnider C, Efron N (2004). Short-term physiologic response in neophyte patients fitted with hydrogel and silicone hydrogel contact lenses. Optom Vis Sci 81:911-921.
|